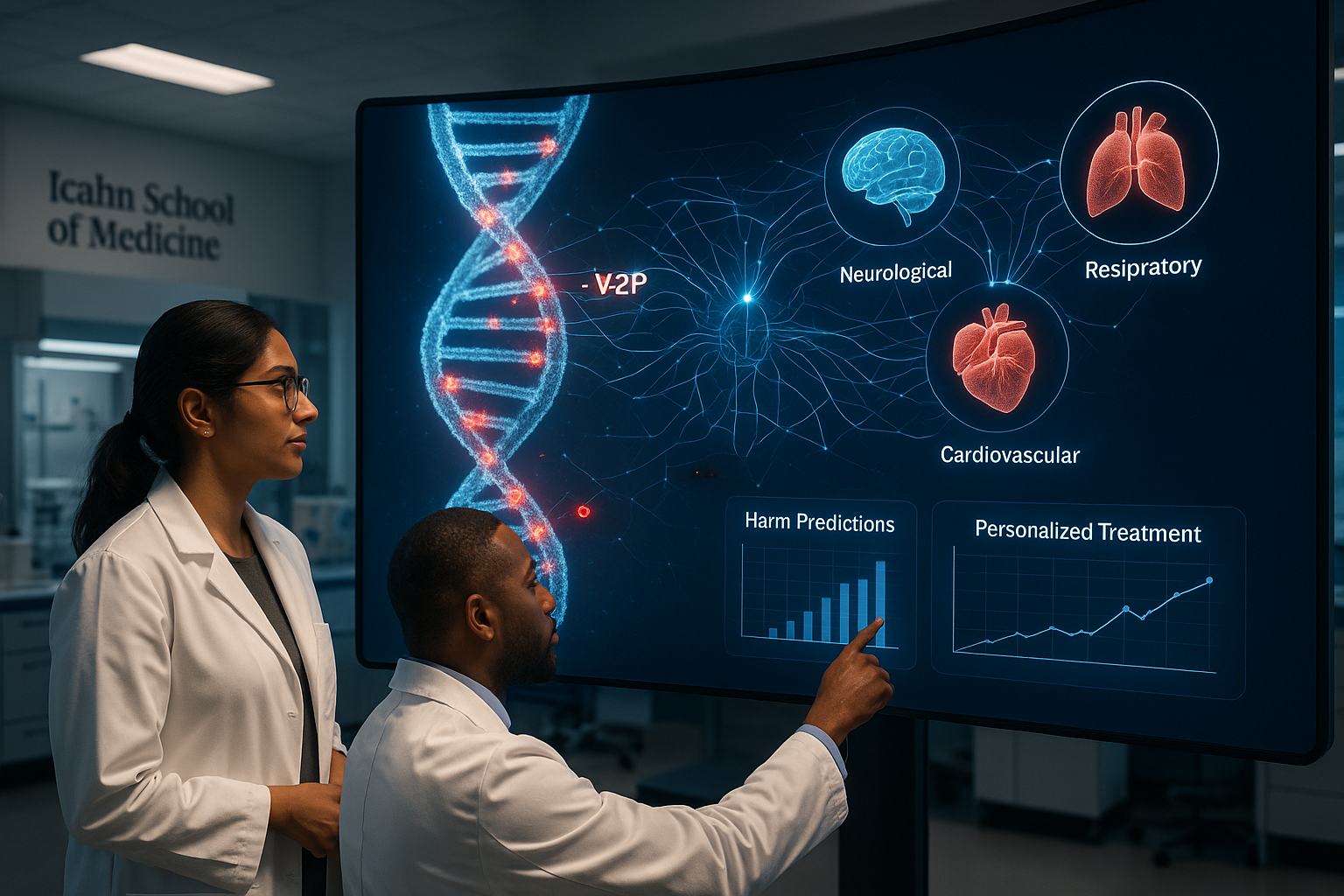
Researchers at the Icahn School of Medicine at Mount Sinai have developed an artificial intelligence system called V2P that not only assesses whether genetic mutations are likely to be harmful but also predicts the broad categories of disease they may cause. The approach, described in a paper in Nature Communications, is intended to accelerate genetic diagnosis and support more personalized treatment, particularly for rare and complex conditions.
Scientists at the Icahn School of Medicine at Mount Sinai have introduced V2P, an artificial intelligence system designed to address a longstanding gap in genetic analysis.
Most existing tools focus on determining whether a mutation is potentially damaging, but stop short of indicating what kind of disease may result. V2P (Variant to Phenotype) is designed to go further by using machine learning to connect genetic variants with their expected phenotypic outcomes — that is, the broad types of diseases or traits a mutation may produce, such as nervous system disorders or cancers, according to Mount Sinai.
The model uses a multi‑task, multi‑output machine-learning framework trained on large datasets of pathogenic and putatively benign genetic variants paired with phenotype information. This training allows it to estimate both whether a variant is pathogenic or benign and which of 23 top-level Human Phenotype Ontology disease phenotype categories it is most likely to affect.
In evaluations that included de‑identified patient sequencing data, V2P frequently ranked the true disease-causing mutation among the top 10 candidate variants in a given case, a result the Mount Sinai team says could help streamline and speed up the diagnostic process.
"Our approach allows us to pinpoint the genetic changes that are most relevant to a patient's condition, rather than sifting through thousands of possible variants," said David Stein, PhD, the study's first author, in a statement released by Mount Sinai. "By determining not only whether a variant is pathogenic but also the type of disease it is likely to cause, we can improve both the speed and accuracy of genetic interpretation and diagnostics."
Co‑senior author Avner Schlessinger, PhD, Professor of Pharmacological Sciences and Director of the AI Small Molecule Drug Discovery Center at Icahn Mount Sinai, highlighted the tool's potential beyond clinical testing. "Beyond diagnostics, V2P could help researchers and drug developers identify the genes and pathways most closely linked to specific diseases," he said. "This can guide the development of therapies that are genetically tailored to the mechanisms of disease, particularly in rare and complex conditions."
At present, V2P sorts mutations into broad disease categories, including disorders of the nervous system and neoplasms (cancers). The research team plans to refine the system so it can make more detailed predictions and to integrate its results with additional data sources, with the goal of further supporting target discovery and drug development.
"V2P gives us a clearer window into how genetic changes translate into disease, which has important implications for both research and patient care," said Yuval Itan, PhD, co‑senior author and Associate Professor of Artificial Intelligence and Human Health at Icahn Mount Sinai. "By connecting specific variants to the types of diseases they are most likely to cause, we can better prioritize which genes and pathways warrant deeper investigation. This helps us move more efficiently from understanding the biology to identifying potential therapeutic approaches and, ultimately, tailoring interventions to an individual's specific genomic profile."
The work, described in the Nature Communications paper "Expanding the utility of variant effect predictions with phenotype-specific models," was led by Stein and co‑authors Meltem Ece Kars, Baptiste Milisavljevic, Matthew Mort, Peter D. Stenson, Jean‑Laurent Casanova, David N. Cooper, Bertrand Boisson, Peng Zhang, Schlessinger and Itan.
According to Mount Sinai, the research was supported by National Institutes of Health grants R24AI167802 and P01AI186771, funding from the Fondation Leducq, and the Leona M. and Harry B. Helmsley Charitable Trust grant 2209‑05535. Additional support came from NIH grants R01CA277794, R01HD107528 and R01NS145483, as well as the Clinical and Translational Science Awards grant UL1TR004419 and infrastructure awards S10OD026880 and S10OD030463.
The study's authors and Mount Sinai researchers say the system advances precision medicine by providing a high‑throughput way to map human genetic variants to likely disease phenotypes, potentially enabling faster, more targeted interventions based on an individual's genetic profile.