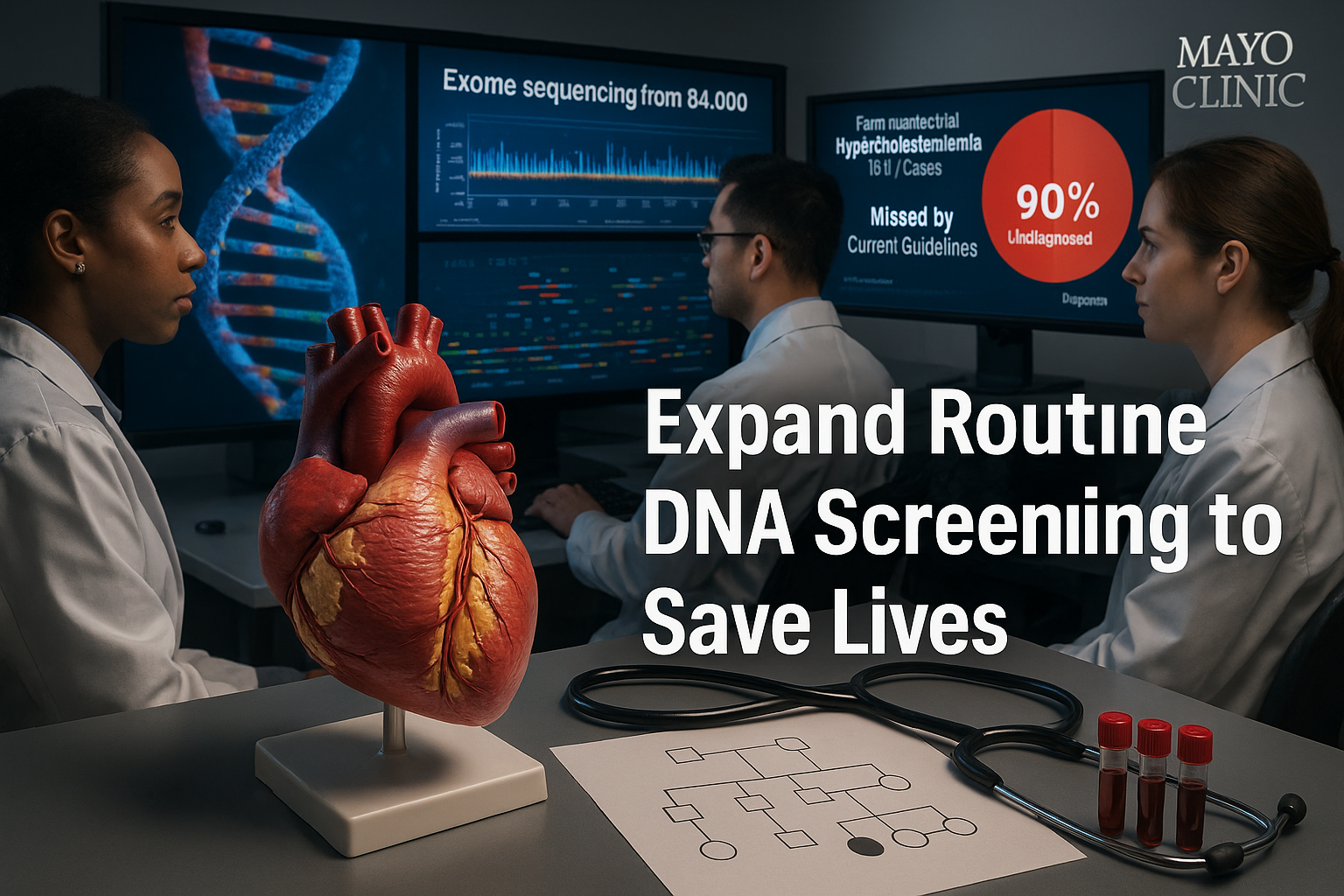
A large Mayo Clinic study reports that current guidelines fail to detect nearly 90% of people with familial hypercholesterolemia, a common inherited cause of dangerously high cholesterol and early heart disease. Researchers analyzed exome data from more than 84,000 participants and found that most would not have been selected for standard genetic testing. Expanding routine DNA screening, they say, could help identify at-risk individuals earlier and prevent severe cardiovascular outcomes.
Familial hypercholesterolemia (FH) is one of the most common genetic disorders, affecting an estimated 1 in 200 to 250 people worldwide. It leads to very high levels of low-density lipoprotein (LDL) cholesterol — often called "bad" cholesterol — beginning at birth, sharply increasing the risk of heart attacks and strokes over a lifetime. Although effective cholesterol-lowering treatments exist, many people with FH remain undiagnosed, and the condition can move quietly through family lines for years.
In a study published in Circulation: Genomic and Precision Medicine, Mayo Clinic researchers used exome sequencing to examine the protein-coding portions of the genome, where most disease-causing mutations occur. More than 84,000 participants at Mayo Clinic locations in Arizona, Florida and Minnesota enrolled through the Tapestry DNA research study, a population-based program designed to bring genomics into routine care.
From this group, the team identified 419 people with genetic variants known to cause familial hypercholesterolemia. According to the Mayo Clinic report on the study, nearly 90% of these individuals would not have been selected for standard genetic testing under existing national guidelines, which rely primarily on cholesterol levels and reported family history. Nearly 75% did not meet current clinical testing criteria, underscoring what researchers describe as a substantial blind spot in prevention efforts.
Roughly 1 in 5 participants with FH-causing variants had already developed coronary artery disease by the time their DNA analysis was reviewed, the study found. That pattern suggests many high-risk patients are not identified until after they develop serious cardiovascular problems.
"Our findings expose a blind spot in current national guidelines, which rely on cholesterol levels and family history to determine who should receive genetic testing," said Niloy Jewel Samadder, M.D., the study's lead author and a Mayo Clinic gastroenterologist and cancer geneticist, in a statement released through Mayo Clinic and ScienceDaily. "If we can find those at risk of cardiovascular disease early, we can treat it early and change its course and likely save lives."
The findings add to Mayo Clinic's broader Tapestry effort, which has generated one of the institution's largest collections of exome data to support individualized care. Tapestry has now sequenced exomes from more than 100,000 participants and is integrating actionable results, including FH-related variants, into electronic health records to guide prevention and treatment.
Mayo Clinic describes this work as central to its Precure strategic priority, which focuses on predicting and preventing serious diseases before they advance. Cardiovascular disease remains the leading cause of death in the United States, and high cholesterol is a major modifiable risk factor. The researchers say that broader, population-based DNA screening for conditions such as familial hypercholesterolemia could dramatically improve early detection and help reduce the long-term burden of heart disease.