Laboratory research led by scientists at Khon Kaen University indicates that cannabidiol (CBD) and delta-9-tetrahydrocannabinol (THC), two key cannabis compounds, can slow the growth and spread of ovarian cancer cells in vitro, particularly when used together in a 1:1 ratio, while causing relatively limited damage to healthy cells. The early-stage findings, reported in Frontiers in Pharmacology, suggest a potential avenue for future ovarian cancer treatments but are far from clinical use.
Ovarian cancer is among the most lethal gynecological cancers, largely because it is often diagnosed at an advanced stage, recurs frequently, and has limited long-term treatment options. A team led by Dr. Siyao Tong of Khon Kaen University investigated whether two cannabis-derived compounds—cannabidiol (CBD), which is non-psychoactive, and delta-9-tetrahydrocannabinol (THC), which is psychoactive—could exert anti-cancer effects on ovarian cancer cells.
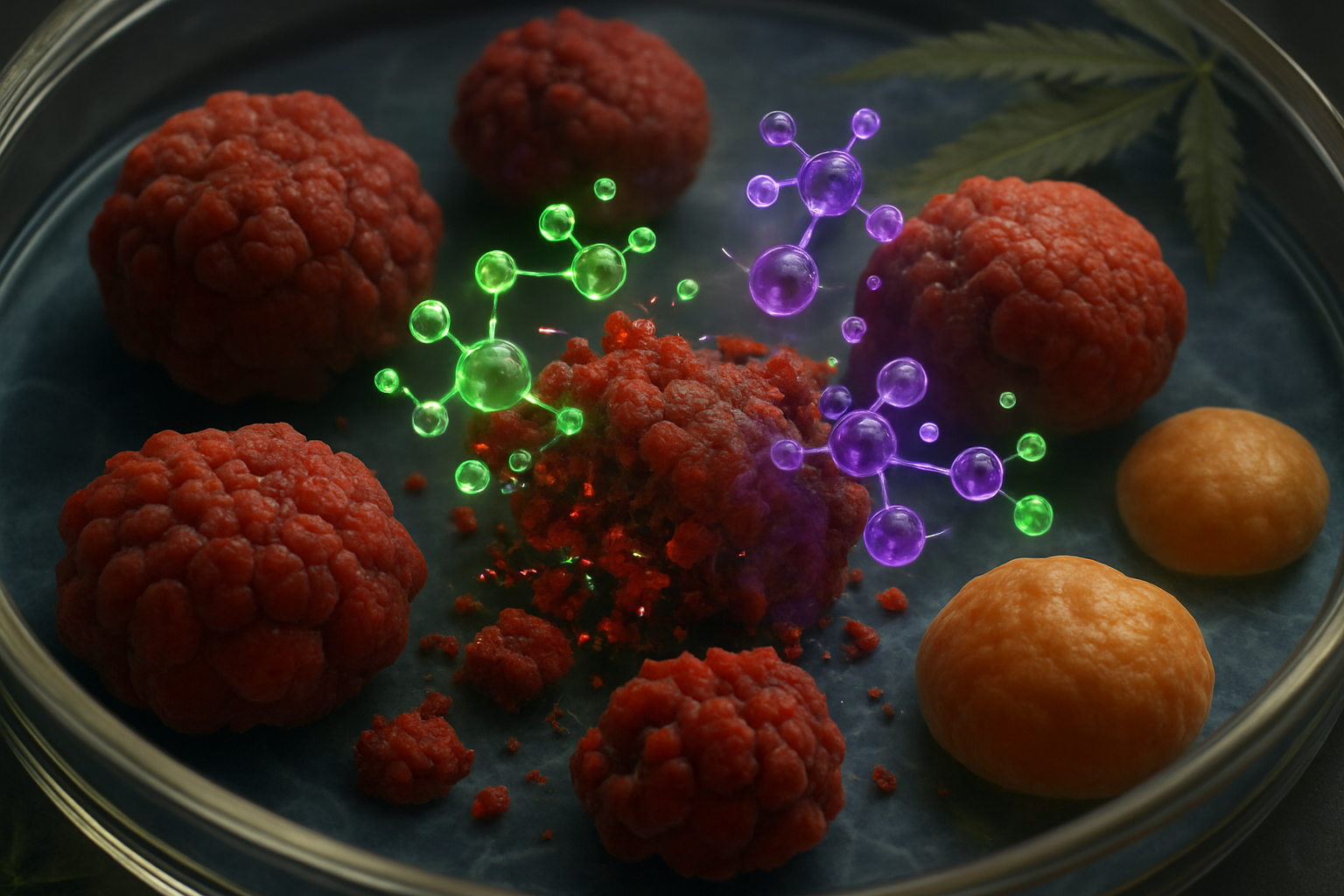
According to a summary from Frontiers relayed by ScienceDaily, the researchers tested CBD and THC on two human ovarian cancer cell lines: one sensitive to platinum-based chemotherapy and one resistant. Both compounds, when applied individually, reduced colony formation and slowed the proliferation of cancer cells. The strongest effects were observed when CBD and THC were combined.
In particular, the team reported that a 1:1 ratio of CBD to THC produced the most pronounced inhibitory impact on cell growth. “Notably, the inhibitory effect was most pronounced when CBD and THC were used in a 1:1 ratio,” Dr. Tong said, as quoted in coverage of the study.
Additional experiments showed that the compounds also reduced the migration of ovarian cancer cells in vitro, a process linked to metastasis, which is a leading cause of death in ovarian cancer. The study further found that both cancer cell lines—platinum-sensitive and platinum-resistant—responded similarly to the treatments, suggesting that the approach might be relevant across different ovarian cancer subtypes.
The researchers also tested the compounds on healthy cells and reported that CBD, THC, and their combination caused relatively little damage to non-cancerous cells at the doses examined. This raises the possibility that therapies based on these compounds could be less toxic and easier to tolerate than many current cancer drugs, though this has not yet been tested in animals or humans.
At the molecular level, the study, published in Frontiers in Pharmacology in 2025, reported that CBD and THC, particularly in combination, appeared to modulate the PI3K/AKT/mTOR signaling pathway, which is often overactivated in ovarian cancer and associated with tumor growth and drug resistance. The authors described a normalization or inhibition of this pathway in treated cells, consistent with decreased cancer cell growth and invasion.
All of the experiments in this work were conducted in vitro, using cultured cells rather than animal models or patients. Dr. Tong and colleagues emphasized that this is an early-stage, preclinical study and that the findings may not fully capture how tumors behave in living organisms. Substantial further research, including in vivo studies and eventually clinical trials, would be required to determine whether CBD- and THC-based regimens are safe and effective for people with ovarian cancer.
For now, the results add to a growing body of laboratory evidence that cannabinoids can exert selective anti-cancer effects against ovarian cancer cells while sparing healthy cells, but experts caution that it is too soon to consider these compounds as established treatments outside controlled research settings.