A large study published in Neurology finds that impaired kidney function is linked to higher levels of Alzheimer’s biomarkers in the blood, without increasing overall dementia risk. However, among people who already have elevated biomarker levels, poor kidney health may hasten when dementia symptoms appear, underscoring the need to factor kidney function into interpretation of Alzheimer’s blood tests.
Published on December 3, 2025, in Neurology, the medical journal of the American Academy of Neurology, the study examined how kidney function relates to blood-based biomarkers of Alzheimer’s disease.
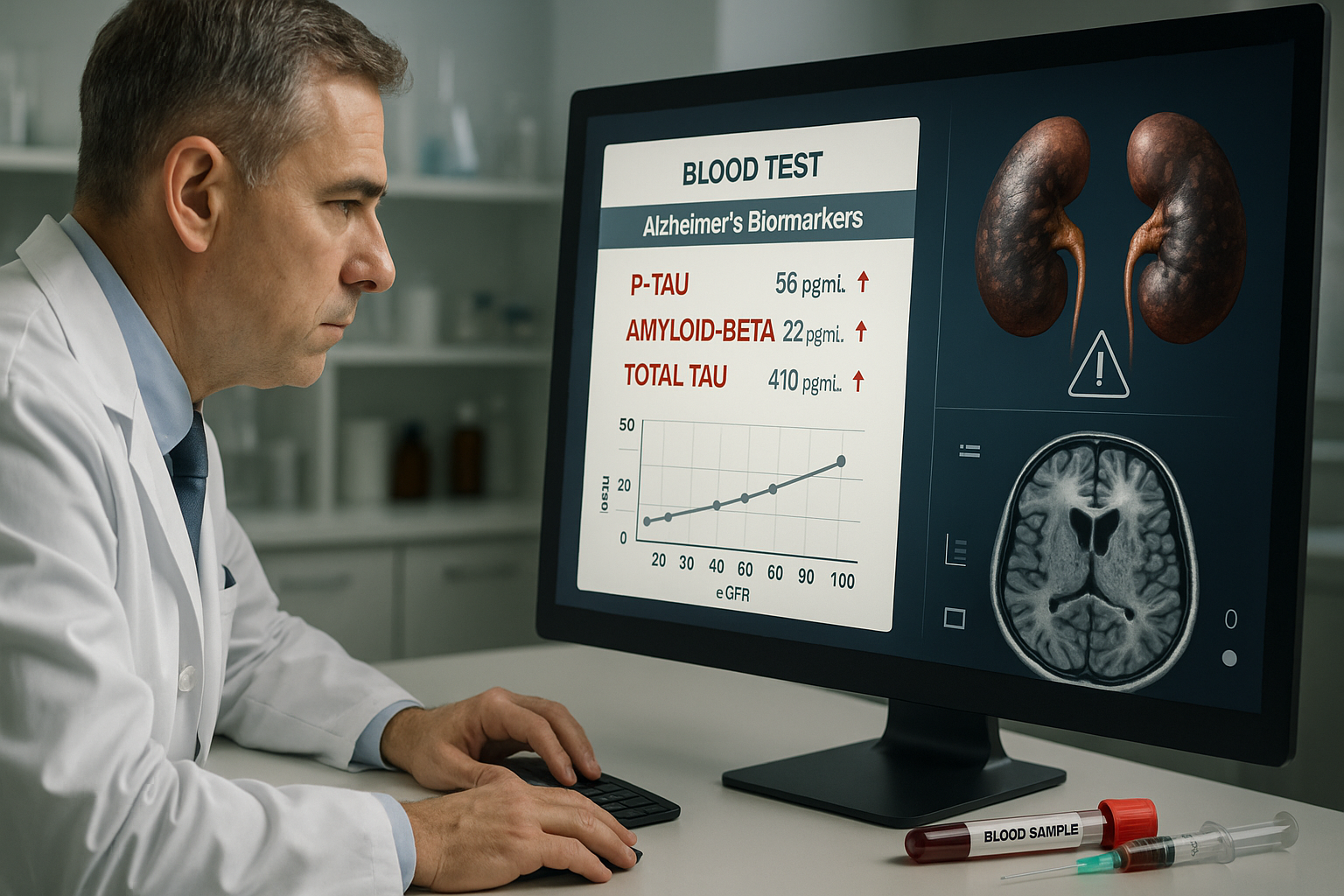
Led by Francesca Gasparini, MD, of Karolinska Institutet in Stockholm, Sweden, the research followed 2,279 community-dwelling adults with an average age of 72, none of whom had dementia at the start of the study. Participants underwent medical examinations, cognitive testing, and blood tests that assessed kidney function and measured several Alzheimer’s-related biomarkers, including tau and amyloid beta proteins, neurofilament light chain (NfL) proteins, and glial fibrillary acidic proteins (GFAP). 【0search1】【0search3】
Over an average follow-up period of about eight years, the researchers divided participants into two groups based on kidney function. Among 1,722 people with healthy kidney function, 221 developed dementia. In the group of 557 people with impaired kidney function, 141 developed dementia. 【0search1】【0search3】
The study found that reduced kidney function was associated with higher levels of most of the Alzheimer’s blood biomarkers examined. However, the authors emphasized that the results show an association rather than proof that poor kidney function directly causes these elevations. Kidneys normally help remove waste and toxins from the blood, which may help explain the link, according to the American Academy of Neurology news release and related coverage. 【0search1】【0search3】【0search8】
After adjusting for factors such as age, sex, and the APOEε4 genetic risk marker for Alzheimer’s disease, the researchers found that impaired kidney function was not linked to an overall increased risk of developing dementia when compared with preserved kidney function. 【0search1】【0search3】
A key finding involved a subgroup of participants with both impaired kidney function and elevated levels of neurofilament light chain. In this group, dementia risk was nearly twice as high as in people who had preserved kidney function but similarly elevated NfL levels, according to the American Academy of Neurology and ScienceDaily summaries. This pattern suggests that kidney health may influence the timing of dementia onset in people who already show signs of neurodegeneration, rather than substantially changing the overall likelihood of developing dementia. 【0search1】【0search3】【0search8】
"Our study found that when the kidneys are not functioning properly, there may be higher levels of Alzheimer’s biomarkers in the blood," Gasparini said. "While we did not find that having reduced kidney function increased the risk of developing dementia, we did find that impaired kidney function may accelerate the onset of dementia in people who have higher levels of biomarkers. This highlights the need for doctors to consider kidney function when interpreting results of Alzheimer’s biomarkers in the blood." 【0search1】【0search3】【0search8】
Gasparini underscored the clinical implications in remarks quoted by the American Academy of Neurology and partner outlets: "When looking at these biomarkers in older adults, keeping an eye on kidney health may be more important than one might think. Monitoring kidney health may help clinicians better interpret these biomarkers and identify who might be at risk for faster disease progression." 【0search1】【0search2】【0search3】
According to coverage by Medical Xpress and other outlets drawing on the Neurology paper, the study had several limitations. Alzheimer’s-related blood biomarkers were measured only once, so the researchers could not examine how changes in kidney function over time might affect biomarker levels. In addition, most participants were highly educated and lived in urban areas in Sweden, which may limit how broadly the findings apply to other populations. 【0search2】【0search3】【0search8】
Overall, the study suggests that in older adults, kidney health can meaningfully influence how Alzheimer’s blood tests should be interpreted, particularly for people with already elevated biomarker levels, even though reduced kidney function alone does not appear to raise overall dementia risk.