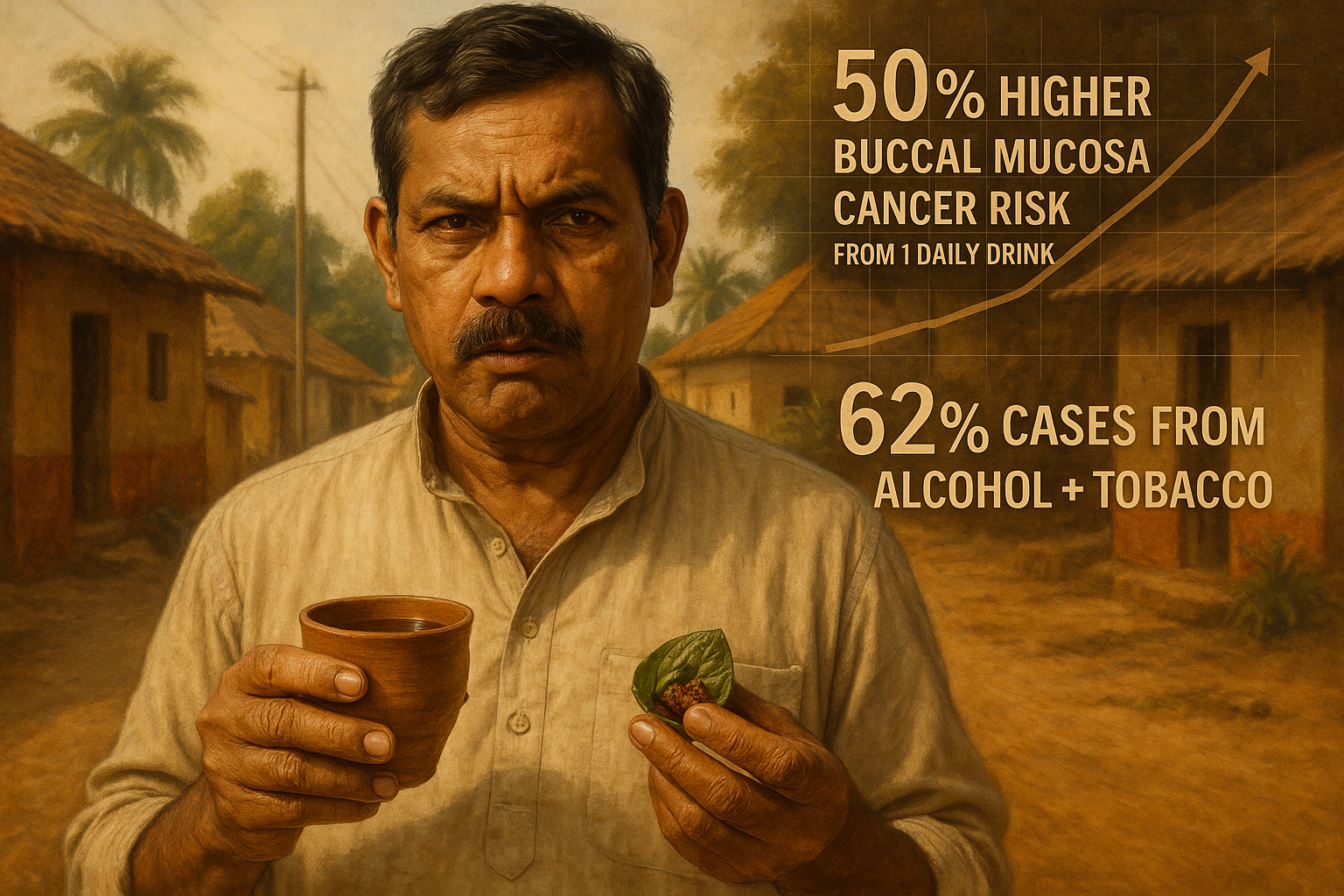
A large case-control study in India reports that drinking about one standard drink a day (roughly 9 grams of alcohol) is associated with an estimated 50% higher risk of buccal mucosa cancer. The researchers also estimate that the combination of alcohol use and chewing tobacco may account for about 62% of cases nationally, with the strongest association seen among people who mainly consumed locally brewed alcoholic beverages.
A large comparative, multicentre case-control study published online in the open-access journal BMJ Global Health found that even low levels of alcohol consumption were associated with a higher risk of buccal mucosa cancer—the most common form of mouth cancer in India.
The researchers compared 1,803 men diagnosed with buccal mucosa cancer with 1,903 controls without the disease. Participants were recruited from five study centres between 2010 and 2021. Most participants were aged 35 to 54, and nearly 46% of cases occurred among people aged 25 to 45, according to the report.
Participants provided detailed histories of alcohol use, including the types of drinks consumed. The study recorded 11 internationally recognised beverages—such as beer, whisky, vodka, rum and “breezers” (flavoured alcoholic drinks)—and 30 locally brewed drinks, including apong, bangla, chulli, desi daru and mahua.
Among the cancer cases, 781 reported drinking alcohol and 1,019 did not. In the control group, 481 reported drinking and 1,420 did not. On average, those with cancer reported a longer history of tobacco use—about 21 years compared with roughly 18 years among controls—and they also reported higher daily alcohol intake, nearly 37 grams compared with about 29 grams.
Compared with people who did not drink, alcohol users had an estimated 68% higher risk of buccal mucosa cancer. The estimated risk increase was 72% among people who mainly consumed internationally recognised drinks and 87% among those who mainly consumed locally brewed alcohol.
The analysis suggested that there was no clear “safe” threshold: drinking under 2 grams of beer per day was still associated with elevated risk, while consuming about 9 grams of alcohol per day—roughly one standard drink—was associated with an estimated 50% increase.
The researchers reported the largest effect when alcohol use overlapped with chewing tobacco. Concurrent exposure was associated with more than a fourfold increase in risk, and the team estimated that the interaction between alcohol and chewing tobacco could account for about 62% of buccal mucosa cancer cases in India. They also estimated that alcohol alone accounts for nearly 11.5% of buccal mucosa cancer cases nationally, rising to about 14% in some high-prevalence states, including Meghalaya, Assam and Madhya Pradesh.
The report noted that mouth cancer is the second most common cancer in India, with an estimated 143,759 new diagnoses and 79,979 deaths each year. Incidence rates are reported to be just under 15 per 100,000 Indian men. Survival outcomes remain poor, with about 43% of patients living at least five years after diagnosis.
As a possible explanation, the researchers suggested that ethanol may alter the fat content of the mouth’s inner lining, increasing permeability and susceptibility to carcinogens present in chewing tobacco products.
The study also flagged concerns about locally brewed alcohol, noting that the market is largely unregulated and that some forms used by participants were reported to contain up to 90% alcohol. The researchers said the higher risk linked to local brews could be partly related to contamination with toxic substances such as methanol and acetaldehyde.
“In summary, our study demonstrates that there is no safe limit of alcohol consumption for [buccal mucosa cancer] risk…Our findings suggest that public health action towards prevention of alcohol and tobacco use could largely eliminate [buccal mucosa cancer] from India,” the authors concluded.