A study of young female university students in Saudi Arabia has found that symptoms of anxiety and insomnia are associated with reduced levels of natural killer cells, key components of the immune system’s early defense. The findings suggest that psychological stressors may be linked to weaker immune responses, though the research shows correlation rather than causation and is limited to a small, specific population.
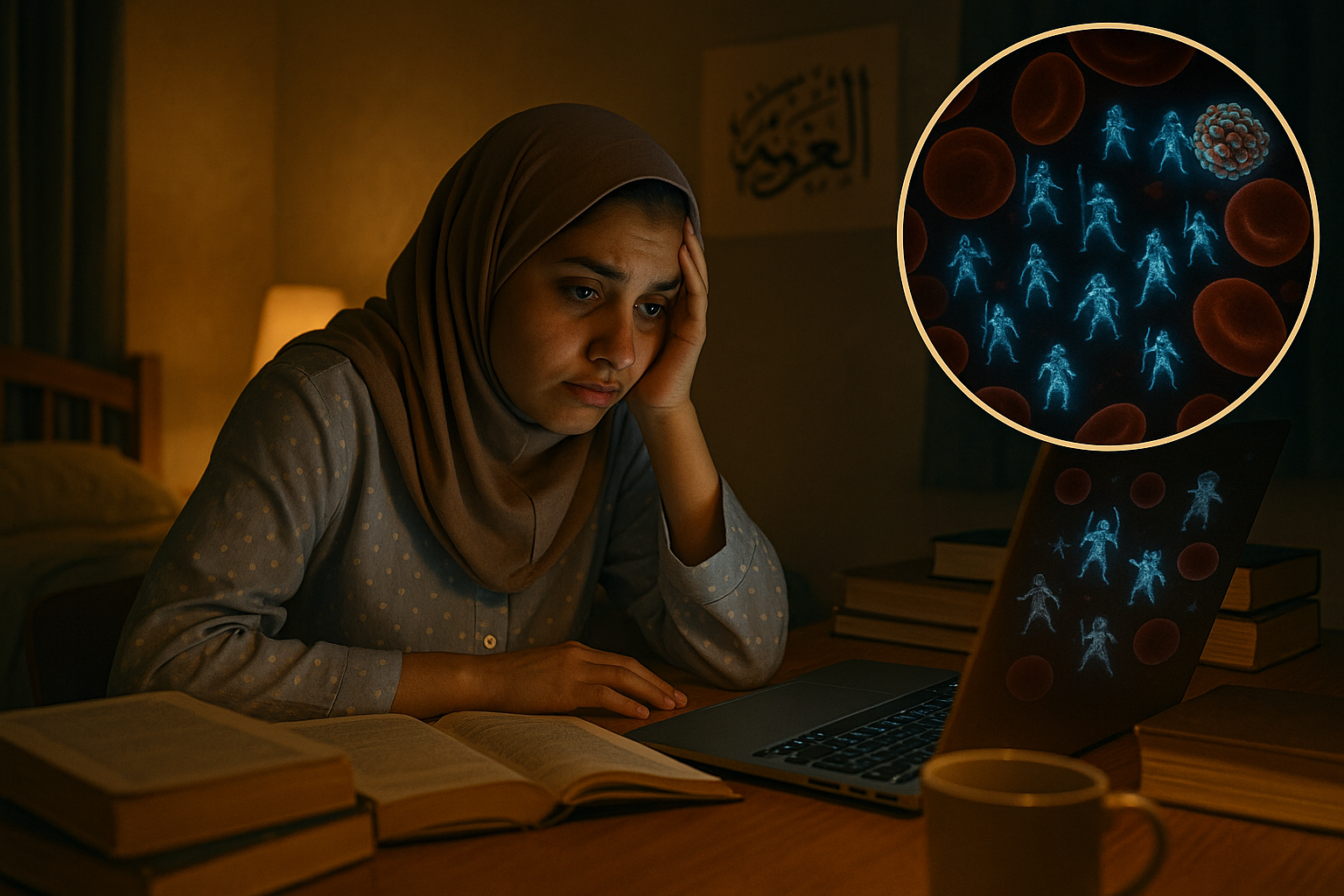
Natural killer (NK) cells serve as part of the immune system's frontline defense, targeting infected or abnormal cells to help prevent the spread of infections and disease. In a recent study published in Frontiers in Immunology, researchers from Taibah University in Madinah, Saudi Arabia, examined how anxiety and insomnia are associated with NK cells among 60 healthy female students aged 17 to 23.
The cross-sectional study, conducted at Taibah University, asked participants to complete questionnaires on sociodemographic factors and validated measures of generalized anxiety (GAD-7) and insomnia symptoms. According to the study, about 53% of the students reported sleep disturbances suggestive of insomnia, while 75% reported anxiety symptoms at varying levels of severity, including roughly 17% with moderate and 13% with severe symptoms.
Blood samples were analyzed to assess NK cell counts and subtypes. The team focused on circulatory NK cells and their two main subpopulations: the cytotoxic CD16+CD56dim cells, which constitute the majority of peripheral NK cells, and the less frequent CD16+CD56high cells, which are involved in cytokine production and immunoregulation.
The results showed that students with anxiety symptoms had a lower percentage and number of circulatory NK cells and their subpopulations compared with students who did not report anxiety symptoms. Severity appeared to matter: students with moderate or severe anxiety had a significantly lower percentage of circulatory NK cells, while those with minimal or mild anxiety showed only a statistically insignificant decline. Among students reporting insomnia symptoms, the number and percentage of total NK cells and their subpopulations were reduced, and higher anxiety scores in this group were negatively associated with the proportion of total peripheral NK cells.
"We found that in students with insomnia symptoms, count and percentage of total NK cells and their sub-populations were declined," said first author Dr. Renad Alhamawi, an assistant professor of immunology and immunotherapy at Taibah University, in a statement released by Frontiers. "Students with general anxiety symptoms, on the other hand, had a lower percentage and number of circulatory NK cells and their sub-populations, compared to symptom-free students."
The authors note that reductions in NK cells can impair immune function, potentially increasing susceptibility to infections, cancers and some mental health conditions, including depression. They suggest that understanding how psychological stressors such as anxiety and sleep disturbance influence the distribution and activity of immune cells, especially peripheral NK cells, may offer insights into mechanisms underlying inflammation and tumor development.
At the same time, the researchers emphasize the limits of their work. The study was cross-sectional and cannot determine cause and effect. It included only young women at a single university in Saudi Arabia, a group in which anxiety and sleep problems have been reported to be rising disproportionately, which restricts how broadly the findings can be generalized. The authors call for larger, longitudinal studies that include different age groups, sexes and regions to clarify how anxiety and insomnia may relate to immune function over time.
Previous research cited by the authors and other experts suggests that lifestyle measures such as regular physical activity, stress management and adequate, consistent sleep may support healthy NK cell activity and overall immune function. However, anxiety and insomnia are complex conditions that involve multiple biological and psychological processes, and the new findings indicate that they may contribute to immune dysregulation and, in turn, to chronic inflammation and reduced quality of life. The study underscores the importance of addressing mental health and sleep in efforts to maintain robust immune defenses.