SereNeuro Therapeutics has reported promising preclinical data for SN101, an induced pluripotent stem cell-based therapy for chronic osteoarthritis pain. The treatment uses engineered peripheral pain-sensing neurons that sequester inflammatory pain factors without transmitting pain signals, while releasing regenerative molecules that may help preserve cartilage, according to data presented at an International Society for Stem Cell Research symposium.
On December 12, at an International Society for Stem Cell Research (ISSCR) symposium in Cambridge, Massachusetts, SereNeuro Therapeutics, a preclinical biotechnology company developing non-opioid pain therapies, unveiled new data on SN101, a therapy derived from induced pluripotent stem cells (iPSCs).
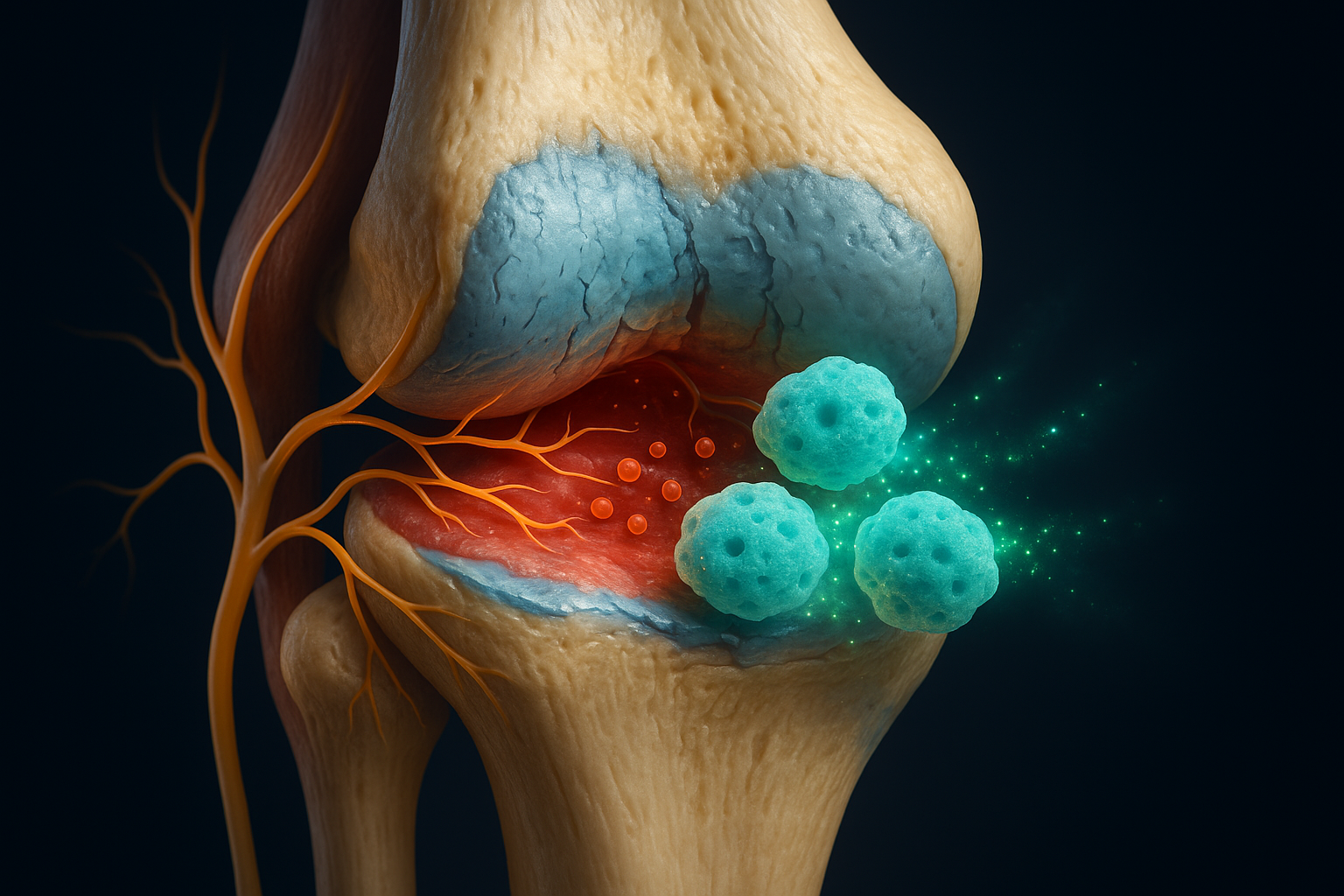
SN101 consists of mature iPSC-derived peripheral pain-sensing neurons, known as nociceptors, and is being developed to treat chronic osteoarthritis joint pain. The approach is positioned as a first-in-class cell-based therapy that departs from traditional pain management strategies.
According to materials from the International Society for Stem Cell Research, SN101 neurons function like a therapeutic "pain sponge" for inflammatory pain molecules. Rather than transmitting pain signals to the brain, the cells sequester inflammatory pain factors locally within the joint, which preclinical data indicate can reduce pain-related signaling. In addition, the neurons secrete mechanistically confirmed regenerative factors, creating an environment that supports preservation of joint tissues and halts cartilage degeneration in preclinical models, positioning SN101 as a potential disease-modifying osteoarthritis drug (DMOAD).
"Our approach utilizes high-purity, iPSC-derived nociceptors (SN101) that effectively function as a sponge for pain factors. By injecting SN101 cells, we counterintuitively relieve pain and halt cartilage degradation," explained Gabsang Lee, scientific co-founder of SereNeuro and a professor of neurology and neuroscience at Johns Hopkins University, in remarks released through ISSCR and partner outlets.
The therapy is distinguished from emerging options such as Nav1.8 ion channel inhibitors, which focus on a single pain-related pathway. By contrast, SN101 cells naturally express a broad array of canonical pain receptors and ion channels, allowing the therapy to influence multiple mechanisms of pain and inflammation simultaneously, according to the ISSCR summary and related news reports.
SN101 is also contrasted with corticosteroid injections, a common standard-of-care treatment for osteoarthritis pain. Corticosteroids can provide short-term symptom relief but have been associated with accelerated cartilage degradation over time.
"Current standard-of-care treatments, particularly corticosteroids, provide temporary relief but are known to accelerate cartilage degradation over time, ultimately worsening the disease," noted Dr. Daniël Saris, a member of SereNeuro's Clinical Advisory Board and a professor of orthopedics and regenerative medicine at Mayo Clinic, in the ISSCR communication.
In preclinical studies summarized by ISSCR and affiliated news releases, SN101 has been shown to ease chronic pain behaviors in animal models while supporting preservation of cartilage and bone structure in treated joints. Because the therapy uses non-opioid, fully mature, non-dividing cells, developers say it is intended to avoid the addiction risks associated with opioid painkillers and to reduce tumorigenicity concerns seen with some proliferative cell therapies.
These findings remain preclinical, and SN101 has not yet entered human trials. Nonetheless, the data highlight a shift toward cell-based, non-opioid strategies that aim not only to relieve chronic osteoarthritis pain but also to protect and potentially preserve joint tissues over time.