A Mount Sinai–led study finds that commonly used heart-attack risk calculators and symptom-based screening fail to identify nearly half of people who will soon experience a first heart attack. The brief report, published November 21 in JACC: Advances, underscores limitations in current prevention strategies and argues for earlier imaging to detect silent plaque.
Researchers from the Mount Sinai Health System analyzed how well two standard cardiac risk tools would have identified patients who went on to suffer a first heart attack.
According to Mount Sinai's summary of the work, the team evaluated 474 individuals under age 66 with no previously known coronary artery disease who experienced a first myocardial infarction. All were treated within the Mount Sinai system. Investigators calculated each patient's 10‑year atherosclerotic cardiovascular disease (ASCVD) risk score and a simulated score from the newer PREVENT calculator, as if the assessments had been performed two days before the heart attack.
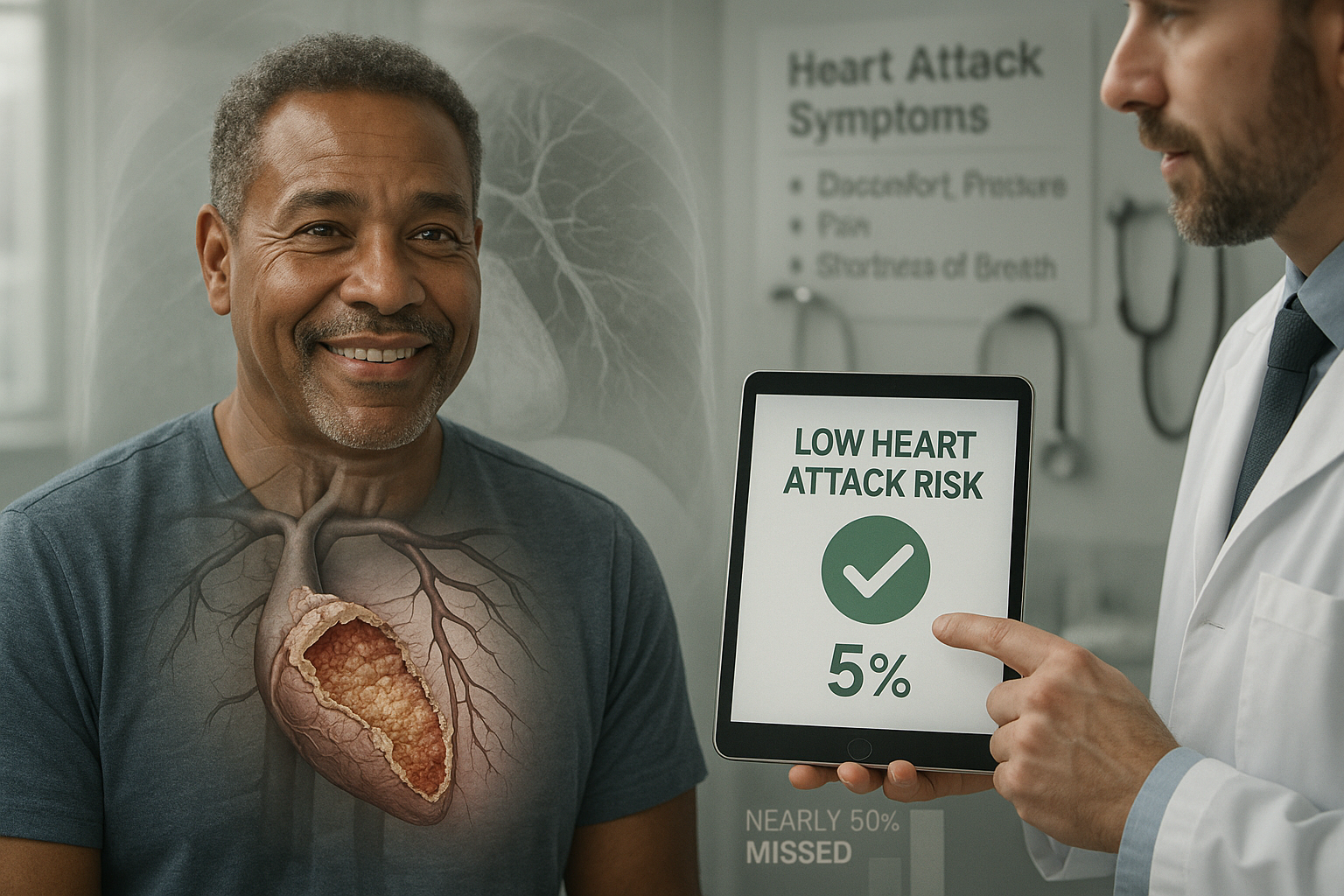
The analysis focused on whether current guidelines would have recommended preventive therapy or further testing. The authors report that, using the ASCVD risk tool, 45 percent of these patients would not have qualified for preventive therapy or additional testing, despite going on to have a heart attack. With the PREVENT equation, 61 percent would have been classified in ranges that did not trigger treatment or further evaluation, even though PREVENT incorporates additional variables beyond age, sex, race, blood pressure, cholesterol, diabetes, and smoking.
The study also examined how close to the event patients developed warning signs. Around 60 percent of participants reported classic symptoms such as chest pain or shortness of breath within 48 hours of their heart attack, meaning that relying on symptoms alone would often leave little time for meaningful intervention.
"Our research shows that population-based risk tools often fail to reflect the true risk for many individual patients," said corresponding author Amir Ahmadi, MD, Clinical Associate Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai, in a statement released by the institution. He noted that if clinicians had evaluated these patients just two days earlier, nearly half would not have been recommended for further testing or preventive therapy under current risk‑based guidelines.
In the same statement, Dr. Ahmadi added that "the current approach of relying on risk scores and symptoms as primary gatekeepers for prevention is not optimal," and suggested it may be time to shift toward atherosclerosis imaging to identify silent plaque before it ruptures.
First author Anna S. Mueller, MD, an internal medicine resident at the Icahn School of Medicine at Mount Sinai, said the findings highlight a mismatch between tools designed for populations and the needs of individual patients. "Our study exposes a major flaw where tools effective for tracking large populations fall short when guiding individualized care," she said. "Instead, doctors should shift their focus from detecting symptomatic heart disease to detecting the plaque itself for earlier treatment, which could save lives."
The brief report, titled "Limitations of Risk- and Symptom-Based Screening in Predicting First Myocardial Infarction," appears in the Journal of the American College of Cardiology: Advances. The authors and Mount Sinai say the results point to a need for refined prevention strategies that incorporate imaging and other methods to better detect high‑risk patients before symptoms appear.