Researchers at Tohoku University report that lubiprostone, a medication commonly used to treat chronic constipation, helped slow the decline of kidney function in patients with chronic kidney disease in a Phase II trial. The findings emerged from work exploring how gut health and constipation influence kidney outcomes.
Chronic kidney disease (CKD) affects people worldwide and often progresses to end-stage kidney failure requiring dialysis, yet there are still no approved drugs that can actively restore kidney function.
A team led by Professor Takaaki Abe at the Tohoku University Graduate School of Medicine investigated an unconventional approach: repurposing lubiprostone, a selective chloride channel activator already prescribed for chronic constipation. Their research builds on prior observations that constipation is common in CKD and is associated with worse kidney outcomes.
"We noticed that constipation is a symptom that often accompanies CKD, and decided to investigate this link further," Abe said in a statement released by Tohoku University. "Essentially, constipation disrupts the intestinal microbiota, which worsens kidney function. Working backwards, we hypothesized that we could improve kidney function by treating constipation."
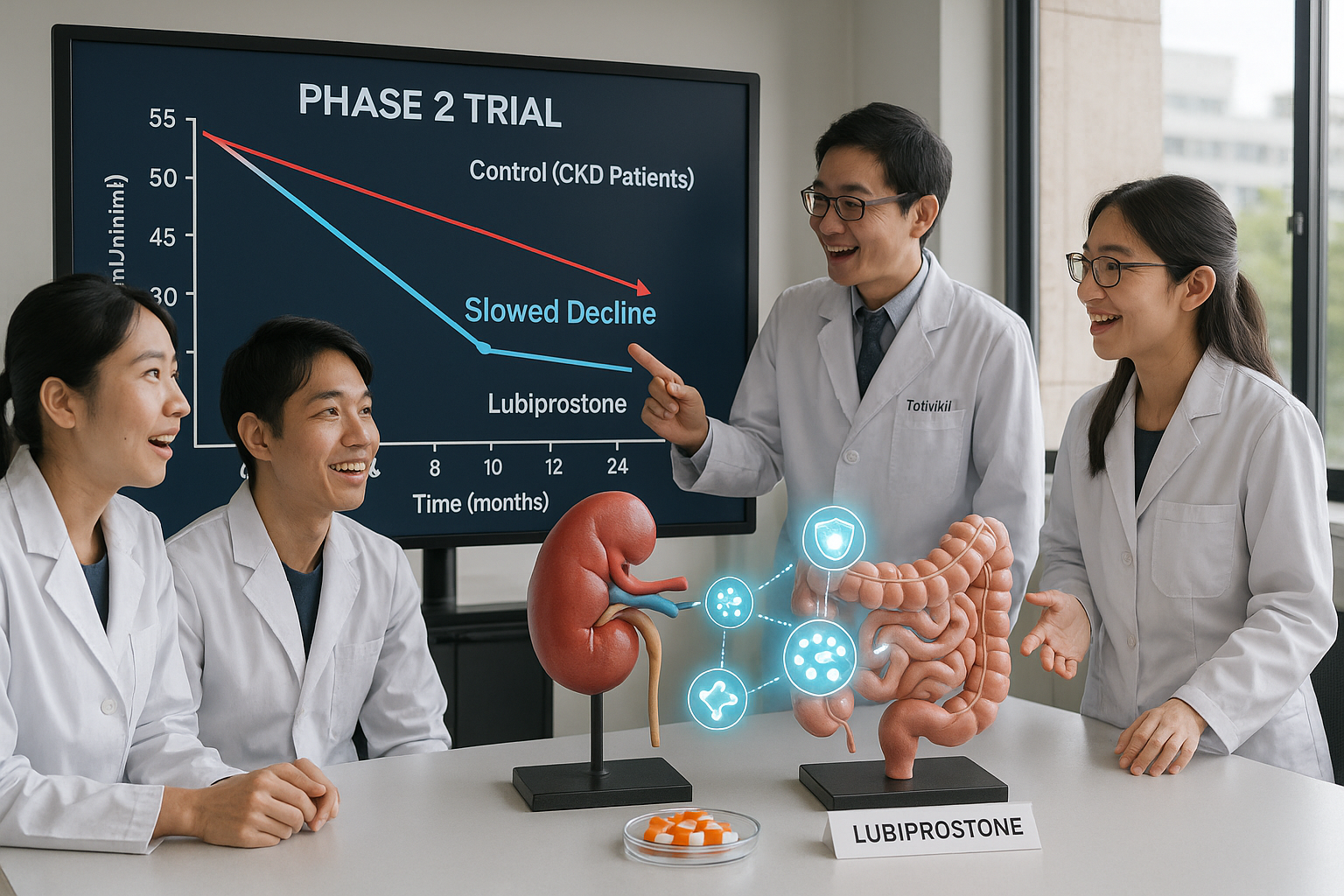
To test this hypothesis, the group conducted the LUBI-CKD TRIAL, a multicenter, randomized, double-blind Phase II study at nine medical facilities in Japan. According to the Science Advances paper and associated institutional releases, the trial enrolled 150 patients with stage IIIb–IV CKD and assigned them to receive either 8 micrograms or 16 micrograms of lubiprostone per day, or a placebo, for 24 weeks.
Kidney function was evaluated using the estimated glomerular filtration rate (eGFR), a standard measure of how well the kidneys filter blood. Compared with participants receiving placebo, those treated with lubiprostone showed a slower decline in eGFR, with the effect most clearly preserved in the 16-microgram group over the 24-week period.
The investigators also explored how the drug exerted this protective effect. Multiomics analyses indicated that lubiprostone modulated gut microbial pathways and increased levels of spermidine, a polyamine compound. The rise in spermidine was linked to enhanced mitochondrial function in kidney tissue, which in turn appeared to have a renoprotective effect by limiting further damage.
The study, published in Science Advances in August 2025, suggests that targeting the gut–kidney axis may offer a new strategy for slowing CKD progression, shifting emphasis from simply reducing uremic toxins to directly preserving renal function through mitochondrial support.
Researchers now plan to validate these findings in a larger Phase III clinical trial and continue the search for biomarkers that could predict which patients will benefit most from this approach. If confirmed, the strategy of using laxatives such as lubiprostone to suppress renal function decline could eventually be extended to other disorders that involve mitochondrial dysfunction, according to Tohoku University and related reports.