Scientists in the U.K. and Canada report the first direct visualization and measurement of alpha‑synuclein oligomers—the small protein clusters long suspected of triggering Parkinson’s—in human brain tissue. Using an ultra‑sensitive imaging method, the team found these clusters were larger and more numerous in Parkinson’s than in age‑matched controls, a result published in Nature Biomedical Engineering that may help guide earlier diagnosis and targeted therapies.
Parkinson’s disease is widely described as the world’s fastest‑growing neurological condition, and about 166,000 people are currently living with a diagnosis in the U.K., according to new prevalence data. Global cases are projected to exceed 25 million by 2050, largely because of population ageing. (pmc.ncbi.nlm.nih.gov)
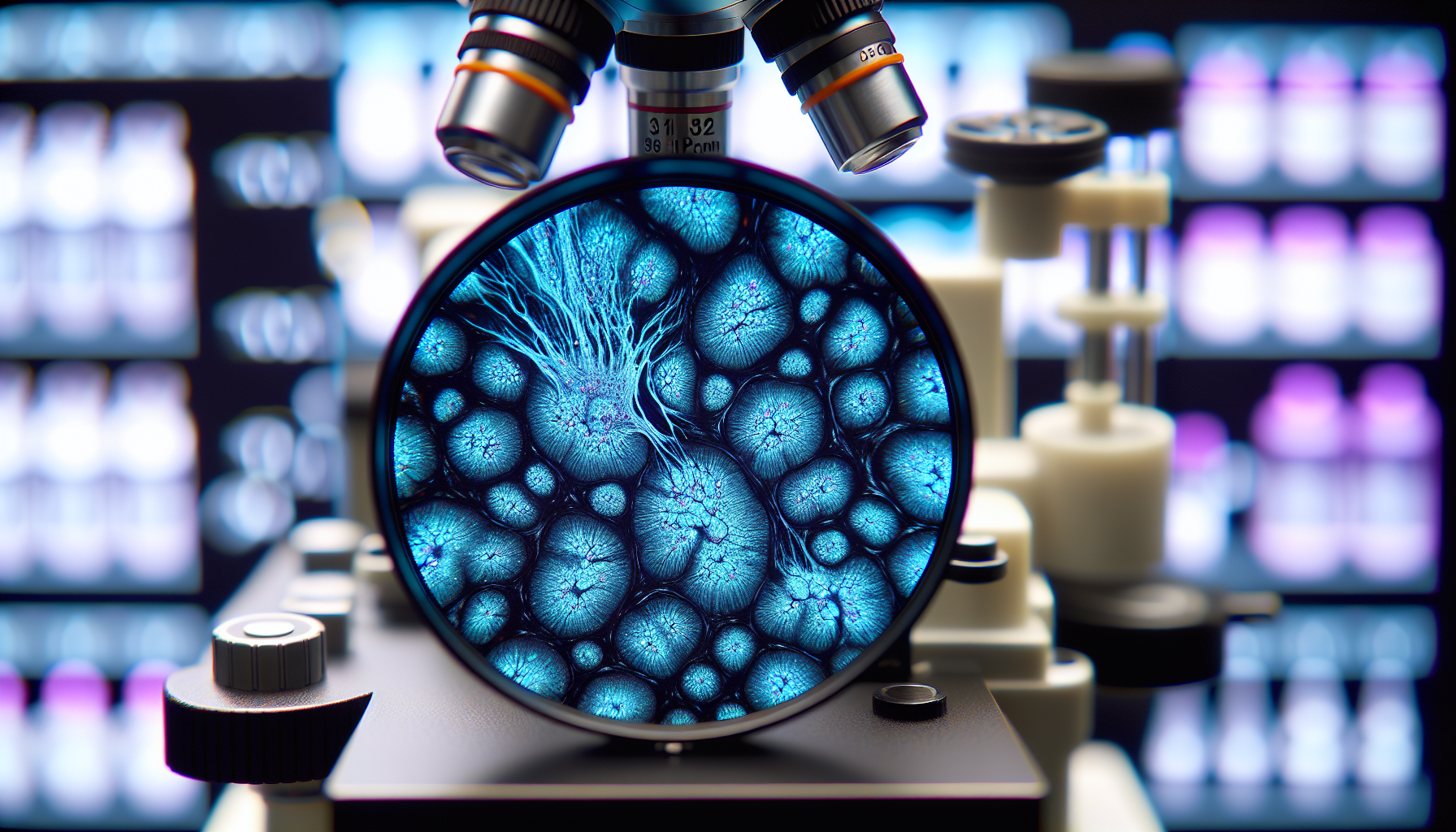
In work led by researchers at the University of Cambridge, UCL, the Francis Crick Institute, and Polytechnique Montréal, scientists developed ASA–PD (Advanced Sensing of Aggregates—Parkinson’s Disease), an optical approach that combines autofluorescence suppression with single‑molecule fluorescence microscopy to map and quantify nanoscale alpha‑synuclein assemblies directly in post‑mortem human brain tissue. The study, published on October 1, 2025, in Nature Biomedical Engineering, reports analysis of more than a million aggregates and identifies a disease‑specific shift in a subpopulation of bright nanoscale assemblies. (dx.doi.org)
“Lewy bodies are the hallmark of Parkinson’s, but they essentially tell you where the disease has been, not where it is right now,” said Steven F. Lee of Cambridge’s Yusuf Hamied Department of Chemistry, a co‑lead author. “If we can observe Parkinson’s at its earliest stages, that would tell us a whole lot more about how the disease develops in the brain and how we might be able to treat it.” (cam.ac.uk)
Examining post‑mortem brain tissue from people with Parkinson’s alongside samples from healthy, similarly aged individuals, the team detected oligomers in both groups. In Parkinson’s, however, the oligomers were larger, brighter and far more numerous, and the researchers observed a subset that appeared only in Parkinson’s cases—potentially an earliest detectable marker of disease. Co‑first author Rebecca Andrews called the new visibility “like being able to see stars in broad daylight.” (cam.ac.uk)
ASA–PD “offers a whole atlas of protein changes across the brain,” said Lucien Weiss of Polytechnique Montréal, who co‑led the work, adding that similar technologies could be applied to other neurodegenerative diseases such as Alzheimer’s and Huntington’s. Sonia Gandhi of the Francis Crick Institute said studying human brain tissue directly is essential to understand “why, where and how protein clusters form” and how they alter the brain environment to drive disease. (cam.ac.uk)
The research underscores the value of donated brain tissue and was supported in part by Aligning Science Across Parkinson’s (ASAP), the Michael J. Fox Foundation for Parkinson’s Research, and the U.K. Medical Research Council, part of UK Research and Innovation. (cam.ac.uk)