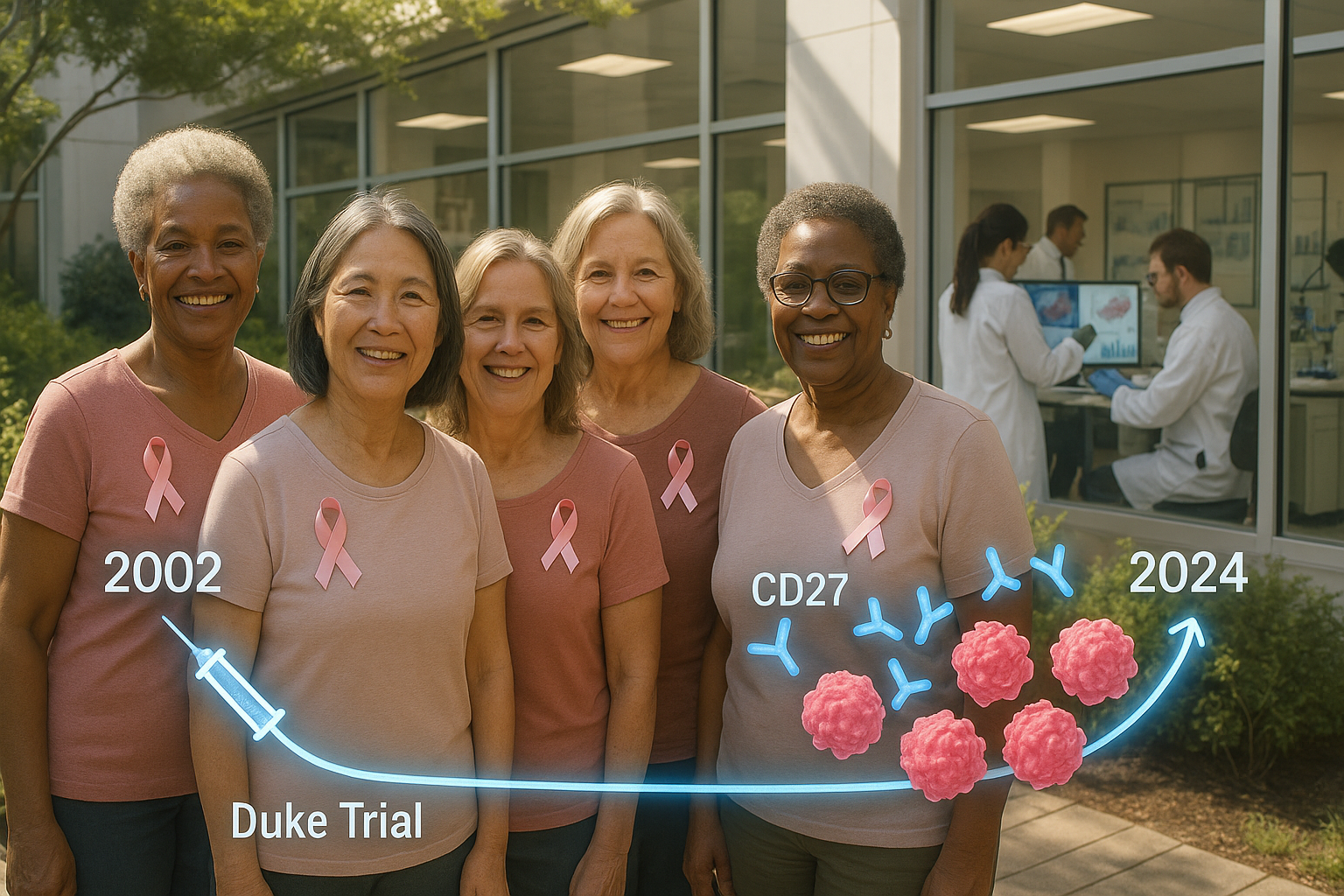
More than 20 years after a small Duke-led clinical trial tested an experimental breast cancer vaccine, Duke Health says all participating women are still alive—an outcome researchers describe as unusual for metastatic disease. Follow-up analyses found long-lived immune cells marked by CD27, and mouse experiments suggest that stimulating CD27 can boost vaccine-driven tumor control.
In the early 2000s, a small group of women with advanced breast cancer enrolled in a clinical trial testing an experimental vaccine led by Herbert Kim Lyerly, M.D., the George Barth Geller Distinguished Professor of Immunology at Duke University School of Medicine.
Duke Health reports that more than two decades later, all participants from that trial are still alive—an outcome the researchers described as extremely uncommon for patients with metastatic breast cancer.
In new work published in Science Immunology, Duke Health scientists led by senior author Zachary Hartman, Ph.D.—an associate professor in the Departments of Surgery, Integrative Immunology, and Pathology at Duke University School of Medicine—re-examined the women’s immune responses years after vaccination. The team found that participants retained immune cells capable of recognizing their cancer, and that these cells shared a marker called CD27, which the researchers described as playing an important role in immune memory.
“We were stunned to see such durable immune responses so many years later,” Hartman said. “It made us ask: What if we could boost this response even more?”
To explore that question, the researchers conducted experiments in mice, combining a vaccine aimed at HER2—a protein found on the surface of some cells, including certain breast cancer cells—with an antibody designed to stimulate CD27. Duke Health said nearly 40% of mice given the combined approach experienced complete tumor regression, compared with 6% of mice that received the vaccine alone.
The researchers reported that the CD27-stimulating antibody increased the activity of CD4+ T cells, often called “helper” T cells. Hartman said these cells are frequently overlooked relative to CD8+ “killer” T cells in cancer research, and argued the findings highlight a larger role for CD4+ cells in sustaining anti-tumor immune memory.
When the team added a separate antibody intended to further support CD8+ T cells, tumor rejection rates in mice rose to nearly 90%, according to Duke Health.
“This study really shifts our thinking,” Hartman said. “It shows that CD4+ T cells aren’t just supporting actors; they can be powerful cancer fighters in their own right and are possibly essential for truly effective anti-tumor responses.”
Duke Health also reported that the CD27 antibody only needed to be administered once, at the same time as the vaccine, to produce long-lasting effects in the mouse experiments—an approach the researchers said could potentially be combined with existing cancer treatments, including immune checkpoint inhibitors and antibody-drug conjugates.
The study was supported by funding from the National Institutes of Health and the U.S. Department of Defense, Duke Health said.
“We’ve known for a long time that vaccines can work against cancer, but they haven’t lived up to the hype,” Hartman said. “This could be a missing piece of the puzzle.”