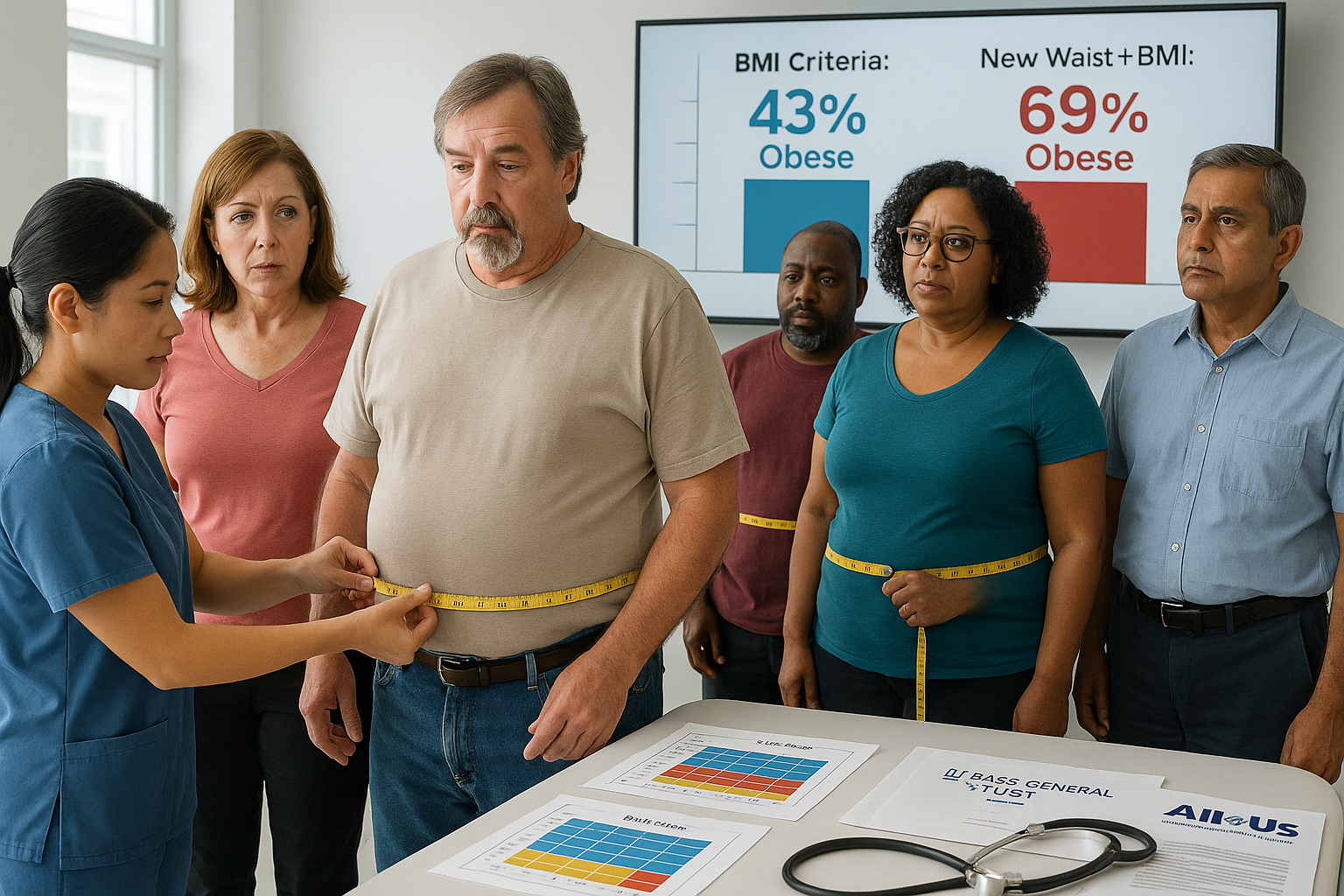
A proposed update to how obesity is defined—combining body mass index with measures of abdominal fat—would raise the share of U.S. adults classified as having obesity from about 43% to roughly 69%, according to a Mass General Brigham analysis of more than 300,000 participants in the National Institutes of Health’s All of Us Research Program.
Researchers at Mass General Brigham report that applying a new diagnostic framework for obesity would substantially increase the proportion of U.S. adults who meet criteria for the condition.
The analysis, published in JAMA Network Open, used data from more than 300,000 participants in the National Institutes of Health’s All of Us Research Program. Under the traditional body mass index (BMI) threshold for obesity, 42.9% of participants qualified. Under the updated framework proposed by a global commission convened by The Lancet Diabetes & Endocrinology, 68.6% met criteria.
What changes under the proposed framework
The proposed approach supplements BMI with anthropometric measures linked to abdominal fat, including waist circumference, waist-to-height ratio, and waist-to-hip ratio. It identifies obesity in two main ways:
- “BMI-plus-anthropometric obesity”: people with a high BMI and at least one elevated anthropometric measure.
- “Anthropometric-only obesity”: people with a BMI in the “normal” range who have at least two elevated anthropometric measures.
The commission’s framework also distinguishes between preclinical obesity and clinical obesity, with clinical obesity defined by obesity-related physical impairment or organ dysfunction.
Mass General Brigham said the commission’s recommendations have been endorsed by at least 76 organizations, including the American Heart Association and The Obesity Society.
Older adults showed the largest increase
Age produced the most pronounced differences in classification. Nearly 80% of adults over 70 met the new criteria in the All of Us analysis.
The rise in prevalence was driven by people classified as having anthropometric-only obesity—individuals who would not have been labeled obese under BMI alone.
Health risks among newly classified individuals
The study found that participants in the anthropometric-only group had higher rates of diabetes, cardiovascular disease, and mortality than participants who did not meet obesity criteria. Roughly half of those who met the new obesity definition were categorized as having clinical obesity.
“We already thought we had an obesity epidemic, but this is astounding,” co-first author Lindsay Fourman, an endocrinologist at Mass General Brigham, said in a statement. She said the findings suggest the medical community will need clearer guidance on which treatment approaches to prioritize for a larger share of the population.
Senior author Steven Grinspoon, chief of Mass General Brigham’s Metabolism Unit, said BMI alone fails to capture body fat distribution and that the elevated risks seen in this newly classified group raise questions about how best to approach treatment, including the potential role of obesity medications.
“Identifying excess body fat is very important,” Fourman said, adding that “Body composition matters — it’s not just pounds on a scale.” The researchers said further work is needed to understand why anthropometric-only obesity develops and which interventions can most effectively reduce abdominal fat and associated health risks.