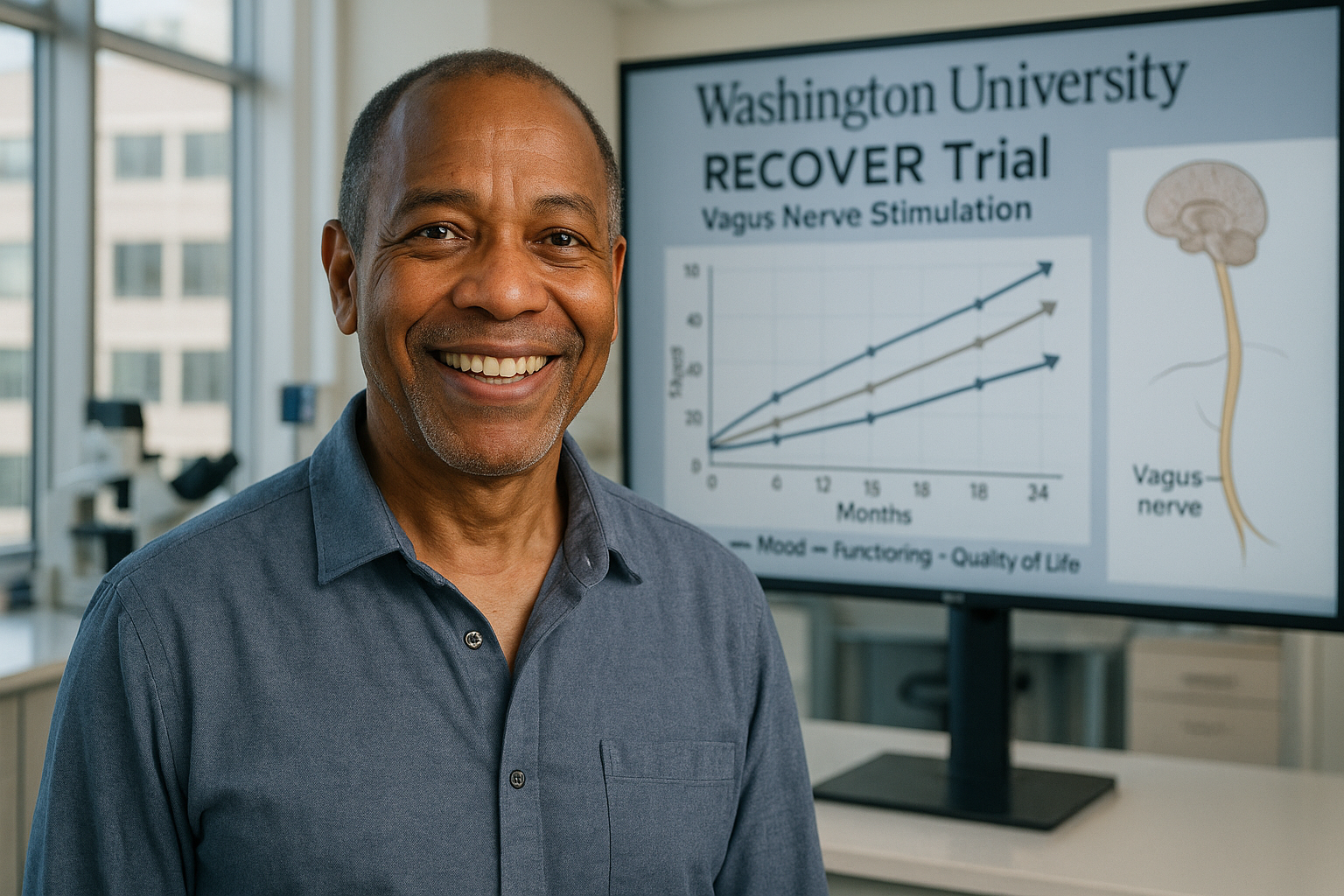
An implanted device that stimulates the vagus nerve was associated with sustained improvements in symptoms, functioning and quality of life among adults with long-standing, treatment-resistant major depression, according to researchers reporting two-year follow-up data from the ongoing RECOVER study led by Washington University School of Medicine in St. Louis.
For people with treatment-resistant depression—when standard medications and psychotherapy do not provide enough relief—new two-year findings from the RECOVER study suggest that adjunctive vagus nerve stimulation (VNS) may deliver durable benefits for some patients.
Researchers at Washington University School of Medicine in St. Louis led the multicenter trial, which enrolled nearly 500 patients across 84 locations in the United States. The VNS approach involves surgically placing a device under the skin in the chest that delivers controlled electrical impulses to the left vagus nerve, a major communication pathway between the brain and internal organs.
The participants represented a highly treatment-resistant group. On average, they had lived with depression for 29 years and had tried about 13 prior treatments, including electroconvulsive therapy and transcranial magnetic stimulation. About three-quarters of participants were unable to work because of their symptoms.
The latest peer-reviewed results were published Jan. 13, 2026, in the International Journal of Neuropsychopharmacology. The paper reports outcomes through 24 months for 214 participants who received active VNS during the first year of the trial and then continued stimulation for a second year.
Rather than focusing solely on symptom scores, investigators assessed depressive symptoms, day-to-day functioning and quality of life, and evaluated how well improvements held up over time. Across multiple measures, the study found that most participants who had reached a prespecified threshold of “meaningful benefit” at 12 months continued to show benefit at 24 months, with median durability at or above roughly 80%. The analysis also found that a substantial share of participants who did not meet criteria for meaningful benefit at 12 months later did so during the second year of stimulation.
“We were shocked that one in five patients was effectively without depressive symptoms at the end of two years,” said lead author Charles R. Conway, MD, a professor of psychiatry and director of the Treatment Resistant Mood Disorders Center at WashU Medicine. Conway said the durability of improvement is notable in a population that typically has low odds of sustained benefit.
The implanted VNS system used in RECOVER is manufactured by LivaNova USA, Inc., which sponsored and funded the study. According to the researchers and the company, a key purpose of RECOVER is to generate evidence that can inform U.S. Centers for Medicare and Medicaid Services (CMS) coverage decisions; CMS has said Medicare coverage is available under a “coverage with evidence development” framework when VNS is provided in a CMS-approved randomized trial.
Major depression is common, with researchers noting that roughly one in five U.S. adults will experience major depression at some point in their lives. In the same report, the researchers said that for as many as one-third of patients, standard antidepressants or psychotherapy do not provide sufficient relief, a pattern often described as treatment-resistant depression.